More Information
Submitted: May 23, 2023 | Approved: August 09, 2023 | Published: August 10, 2023
How to cite this article: Founmilayo LFT, Nadia FF, Polycarpe K. Impact of Moringa oleifera Leaf Flour supplement on Weight Gain in Moderately Acutely Malnourished Children in Benin. Arch Food Nutr Sci. 2023; 7: 070-077.
DOI: 10.29328/journal.afns.1001052
Copyright License: © 2023 Founmilayo LFT, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Anthropometric; Children under five; Complementary food; Moderately acute malnutrition; Moringa oleifera leaf flour; Nutrition education
Impact of Moringa oleifera Leaf Flour supplement on Weight Gain in Moderately Acutely Malnourished Children in Benin
Laleye Flora Tinouade Founmilayo*, Fanou Fogny Nadia and Kayode Polycarpe
School of Nutrition and Food Sciences and Technologies, Faculty of Agronomic Sciences, University of Abomey, Calavi, 01 BP 526, Cotonou, Benin
*Address for Correspondence: Laleye Flora Tinouade Founmilayo, School of Nutrition and Food Sciences and Technologies, Faculty of Agronomic Sciences, University of Abomey-Calavi, 01 BP 526, Cotonou, Benin, Email: [email protected]
In developing countries, malnutrition represents a public health problem, which affects many children under five, during their complementary feeding period. One way to overcome this problem is through the supplementation of complementary flours with locally available food resources, such as Moringa oleifera leaf (MOL). An experimental study was conducted from June through November 2019 in the southern-Benin, with moderately acutely malnourished (MAM) children, using a porridge made of a mixture of corn, malted sorghum, soybean, peanut, milk, and moringa leaf powder. A total of 150 MAM children aged 12-59 months were recruited and divided into two groups, an intervention group (48) and a control group (75). The intervention group received the test food, a porridge made of maize flour supplemented with Moringa oleifera leaf flour (MOL-flour), at least 5 times/week for 6 months. The control group, whose mothers received nutritional education sessions on food diversification as well as the different ways of preparing MOL meals. Sensory evaluation, anthropometric and dietary diversity data were collected. Z-scores Weight/Height, Weight/Age et Height/Age were determined before and right after the intervention. Results showed that 70% of the children and more than 75% of the mothers assessed the porridge as palatable. A significant average weight gain of 1.720 g (p < 0.005) was observed in the intervention group at the end of the experimentation, with a reduction of the prevalence of underweight by 1,33% (p > 0.05), and the number of acute Malnutrition children by 10,42% (p < 0.005).
Malnutrition arises as a direct consequence of poor and inadequate diet [1-5] and affects most children under five in developing countries. In Benin, the prevalence of malnutrition remains high and is a persistent public health problem. Undernutrition affects particularly children under five [6,7] during their complementary feeding period [8-13] and is responsible for half of all child deaths [14]. In fact, 5% of children under five are wasted, 32% suffer from stunted growth, and 17% are underweight [4]. It has been observed that the pathological conditions of malnutrition are closely linked to inappropriate complementary feeding practices [14].
Complementary foods for infants are usually flour-based porridges, which composition varies by nutritional content and age group [10]. According to Kouton, et al. [15], in rural areas, locally-produced porridges do not meet the requirements for most nutrients, have low nutritional value, are often consumed once a day, and are exclusively made with corn.
To address these inadequacies, a number of intervention strategies have been tried in Benin. These are specific nutritional interventions implemented at the community level and using nutrition-rich interventions favorable to the goal of improving the food security environment [16-19]. Among the successful interventions, particular attention has been paid to the use of local food resources to fortify the single staple-based flour. In that regard, Chadare, et al. [20] have provided an extensive list of very relevant local food resources, including Moringa oleifera leaf, which is widely available in Benin.
Moringa oleifera leaf (MOL) is an important local food resource for rural African communities. It is used as a food supplement for different age groups thanks to its high nutritional value [11,13,19,21-26]. Across many developing countries, MOL is used as supplementary food for the fortification of infants and children [9,11,12,22-24,27]. They are known to provide seven times more vitamin C than oranges, 10 times more vitamin A than carrots, and 17 times more calcium than milk [28]. Furthermore, MOL is nine times more protein-rich than yoghurt, contains 15 times more potassium than bananas, and has 25 times more iron than spinach [28].
In addition, several studies report the importance of MOL in the fight against malnutrition. As an example, nutritional interventions using 15 g of MOL flour added to the child’s diet (made of porridge, salad, gravy, or rice) for a period of 2 months have shown significant weight gain in children suffering from overall acute malnutrition in India [19]. As well, in the Republic of Benin, a daily intake of 10 g of MOL flour for a period of 6 months in moderately acutely malnourished children aged 6 months to 30 months has been shown to be associated with a significant improvement in their nutritional status [23]. In addition, interventions using MOL-flour-fortified formulas have been shown to improve the nutritional status of children as quickly as interventions based on the consumption of endogenous foods [29].
Also, flours available on the markets are, for the most part, financially and/or geographically out of the reach of households with limited resources, and the promotion of financially-affordable infant formulas such as the one tested in this experimentation is one of the best ways to improve both accessibility and the nutritional status of those children [13]. In fact, this strategy is increasingly promoted as a cost-effective way to improve the nutritional status of children. However, the combined approach of conventional local staple foods fortified with micronutrient-rich endogenous resources is still needed to ensure adequate and sustainable micronutrient nutrition for children [30]. This research is the experimental phase of the FortiMoringa project and aims at determining the nutritional potential of porridge fortified with the micronutrient-rich endogenous food resource such as Moringa oleifera leaf.
In this experimentation, the testing of the effectiveness of the combination of a conventional local staple food (porridge) fortified with a micronutrient-rich endogenous food resource (MOL-flour) in improving the nutritional status of malnourished children was conducted in the town of Aplahoue, southern Benin. The research is carried out within the framework of the FortiMoringa project, which aims at valorizing MOL for better human nutrition.
Study design
The present study represents the experimental phase of the FortiMoringa project, a multi-partner action research project that has been implemented in several focal packages addressing the MOL value chain. It is a longitudinal experimental study with children aged 12 through 59 months who have been screened for mild-to-moderate malnutrition. The study took place in the southern part of Benin (Commune of Aplahoue, Couffo Department) where the rate of food insecurity varies from moderate (14.9%) to severe (1.3%) [31] and represents the highest percentage (38%) of children with stunted growth [32].
Participants and sampling
The subjects targeted in the present study were children aged 12 through 59 months. An initial screening of the children for malnutrition was conducted to identify those who were moderately acutely malnourished (MAM) without complication. Children with a disease such as diabetes, hypertension, and sickle cell were rejected. A sample size of 150 children obtained with G-Power 3.1.9.7 software [33], was estimated sufficient for detecting the smallest difference in weight with a confidence interval of 95%, a test power of 80%, and a non-response rate of 4% [34]. The sample of 150 children was divided into two groups of 75 children, each one being the intervention group and the other being the control group.
The intervention group received the test food, a porridge made of maize flour supplemented with Moringa oleifera leaf flour (MOL-flour), at least 5 times/week for 6 months. On the other hand, the mothers of the children in the control group received nutritional education sessions on food diversification as well as on the different methods of preparing MOL sauce. The National Health Research Ethics Committee (CNERS) of Benin approved the protocol before implementation. The children’s parents were informed and their informed consent was obtained before the start of the study. The experiment was implemented and monitored by a team of six trained nutrition assistants, under the oversight of two supervisors and the general supervision of a principal investigator.
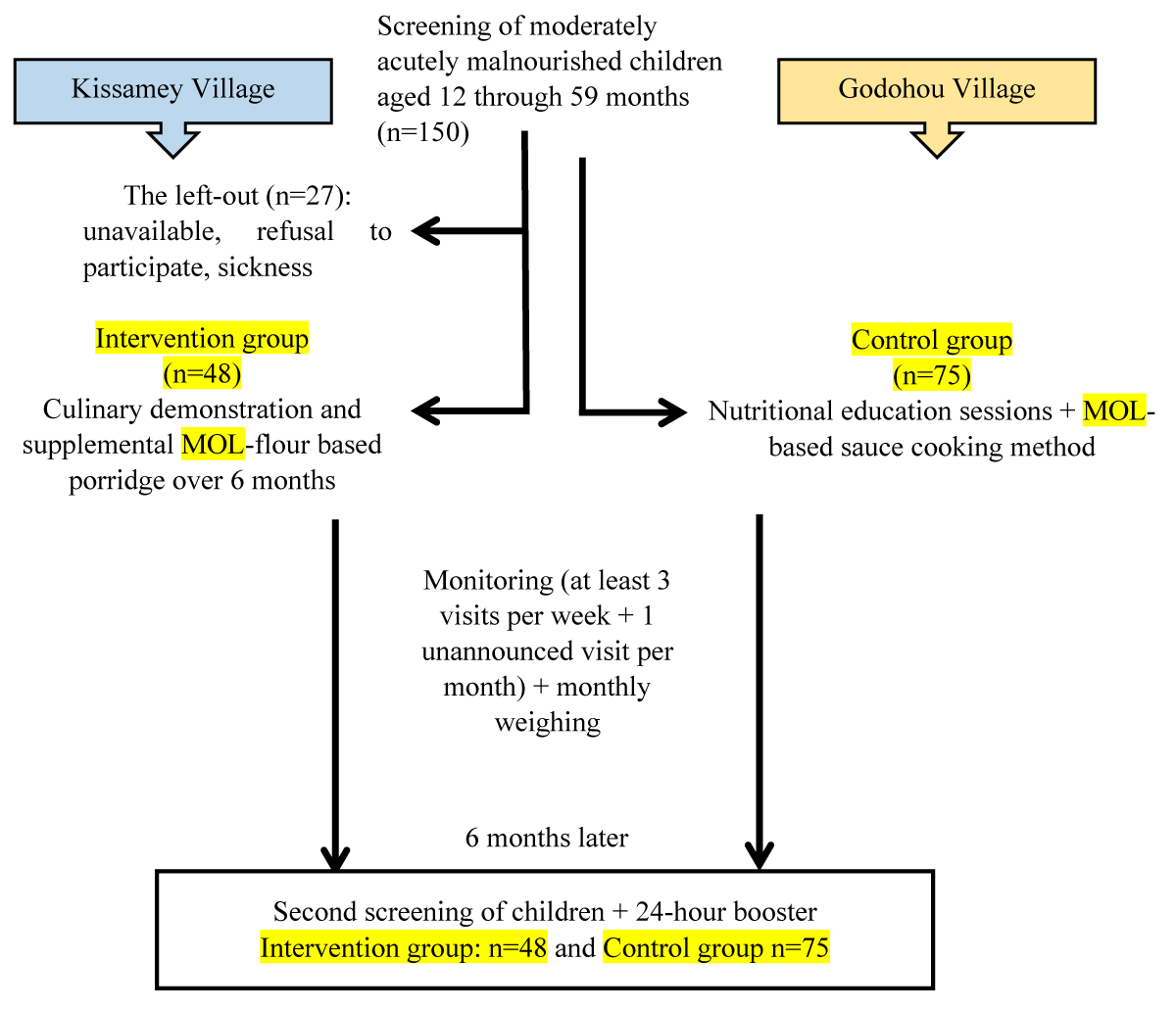
Experimental design
The study’s experimental design is shown in Figure 1. At the beginning of the study, a cooking demonstration was organized with the intervention group in order to train the mothers/guardians in the various steps involved in cooking porridge and to raise their awareness about the benefits of MOL. In addition, children were dewormed with a dose of 200 mg of albendazole before the experiment. During the study, a follow-up consisting of three visits per week and one unannounced visit per month was carried out. To this end, sensory acceptability monitoring and compliance logbooks were used to ensure compliance with the steps prescribed in cooking porridge as well as with the frequency of consumption of the porridge by the children. After 6 months, a second and final screening of the children for malnutrition was conducted in both groups.
Figure 1: Diagram of the experiment.
Test feed
Moringa oleifera leaf-flour-based porridge was the test feed. The MOL-flour formula was developed in the Laboratory of Valorization and Food Bio-ingredient Quality Management (LaBio) at the Faculty of Agronomic Sciences, University of Abomey-Calavi, within the framework of the FortiMoringa project. The flour is made up of 11% cleaned whole corn (Zea mays) to which the following have been incorporated: 30% malted sorghum (Sorghum bicolor), 25% soy (Glycine max) roasted and dehulled, 8% peanut (Arachis hypogeaea) husked and dehulled, 10% MOL-flour, and 15% powdered milk. The formula was developed based on 100 g of dry matter and the MOL-flour nutritional content is 437.09 Kcal, 24.15% proteins, 15.80% lipids, and 4.67% minerals. A serving size of 70 gm of flour was used in preparing the porridge for a single child using 25 cL of boiled drinking water. Simultaneously, 5 tablespoons of flour were diluted in 20 cL of water at room temperature. Then, the diluted flour was poured into the boiling water while stirring, to avoid the formation of lumps. The mixture was cooked over low heat for 10 to 15 minutes, stirring constantly. In this experiment, the children’s mothers or guardians in the intervention group received three 780 g flour packages per week for 6 months.
Sensory analysis
Mothers and children carried out a hedonic test on the MOL-flour-based porridge in order to determine the degree of acceptability. A panel of mothers with at least one child, different from those who participated in the experiment, was asked to evaluate the porridge. A 5-step scale, ranging from 1 (Dislike a lot) to 5 (Like a lot) was used to assess the consistency, color, and taste of the porridge. The children’s facial expression was also noted upon tasting [35].
Anthropometric and food consumption measurements
Weight measurement: We’ve recorded the weight of each child according to standard procedure [36]. Children were undressed before weight measurements. Measurements were taken with a SECA electronic scale, with a maximum range of 150 kg and an accuracy of 100 g on a flat surface. The scale was standardized with a standard weight of 5 kg before the start of the study and was recalibrated every time three children have been weighed. Each child was weighed three times in succession and the average of the three measurements was recorded as that child’s weight. For children under 2 years of age or those who could not stand on their own, their weights were taken using the “double weighing” technique.
Height measurement: The height of each child was determined according to standard procedure [36], using a portable wooden Unicef height gauge (UNICEF Supply Division). It can be placed horizontally or vertically to measure the height of the child while the latter is standing or lying down. Children over 2 were measured standing upright, unshod, with feet together and in such a way that heel, calf, and buttocks touched the wall. The head was held upright. Children under two years of age were laid flat on a board with the head upright and the feet in a vertical position, the sole of the feet flat against the base of the measuring device. Children under 2 were measured lying down because they are agitated and cannot stand still for an upright measurement, and then 0.7 cm was subtracted from the observed measurement before it was recorded on the data collection form.
Age measurement: The ages were recorded directly from an official document (civil status documents, vaccination record, mother’s health record) or were given by the parents. In the absence of these documents, the age is estimated with the help of the mother based on specific events that would have taken place around the time of the child’s birth, using the known sequence of local events. Otherwise, the age is estimated by referring to other children having a birth certificate and being born during the same period in the same household or in the immediate surroundings of the child being surveyed.
Indices: The weight-for-age, weight-for-height, and height-for-age indices were calculated based on references from the WHO and given as z-score [37].
Statistical analysis
Data were collected using the ODK (Open Data Kit) software from which the questionnaires were digitized. To assess the nutritional status of the children, the anthropometric indices (z-score) were calculated and processed using the WHO’s Anthro 3.2.2 software. Excel spreadsheet and SPSS software were used for data processing and analysis. The tests are considered significant at the 5% probability level.
Characteristics of the children
Of the 150 children enrolled at the onset of the study, 123 have completed it (75 children in the control group and 48 in the intervention group) as shown in Table 1. Children were split by sex in both groups: 36% and 55% of the children were girls in the control and intervention groups, respectively. Children in the intervention group were significantly older (30.53 months) than those in the control group (24.82 months), (p ˂ 0.05). The weight and height of the children in both groups did not vary significantly (p > 0.05). In fact, their weight and height were 10.64 kg and 80.76 cm in the control group and then 10.96 kg and 83.06 cm in the intervention group. The mean z-score of the weight/height index was not significantly different between groups (p > 0.05). However, a significant difference was observed between both groups in terms of the mean z-scores of the children’s weight/age and height/age indices (p ˂ 0.05). The z-scores of the weight/age index of the control group (-1.02) were higher than the one for the intervention group (-1.49). As for the height/age index, the best indices were obtained with the control group (-1.24) as compared to the intervention group (-2.26).
| Table 1: Characteristics of the children. | ||||
| Feature | Control (n = 75) | Intervention (n = 48) | P - value | |
| Gender | Boy | 31 (64.58%)a | 36(54.67%)a | 0.106 |
| Girl | 17(36.01%)a | 47(55.03%)a | ||
| Age (months) | 24.82 ± 1.84a | 30.53 ± 1.36b | 0.002 | |
| Weight (kg) | 10.64 ± 0.38a | 10.96 ± 0.29a | 0.579 | |
| Height (cm) | 80.76 ± 2.08a | 83.06 ± 0.94a | 0.555 | |
| Z-score Weight/Height | -0.45 ± 0.16a | -0.35 ± 0.14a | 0.734 | |
| Z-score Weight/Age | -1.02 ± 0.14a | -1.49 ± 0.11b | 0.009 | |
| Z-score Height/Age | -1.24 ± 0.23a | -2.26 ± 0.08b | 0.000 | |
| Values that are followed by the same letter on the same line are not significantly different at the 5% level. n = number of children who participated in the study. | ||||
Sensory evaluation of the MOL-flour-based porridge
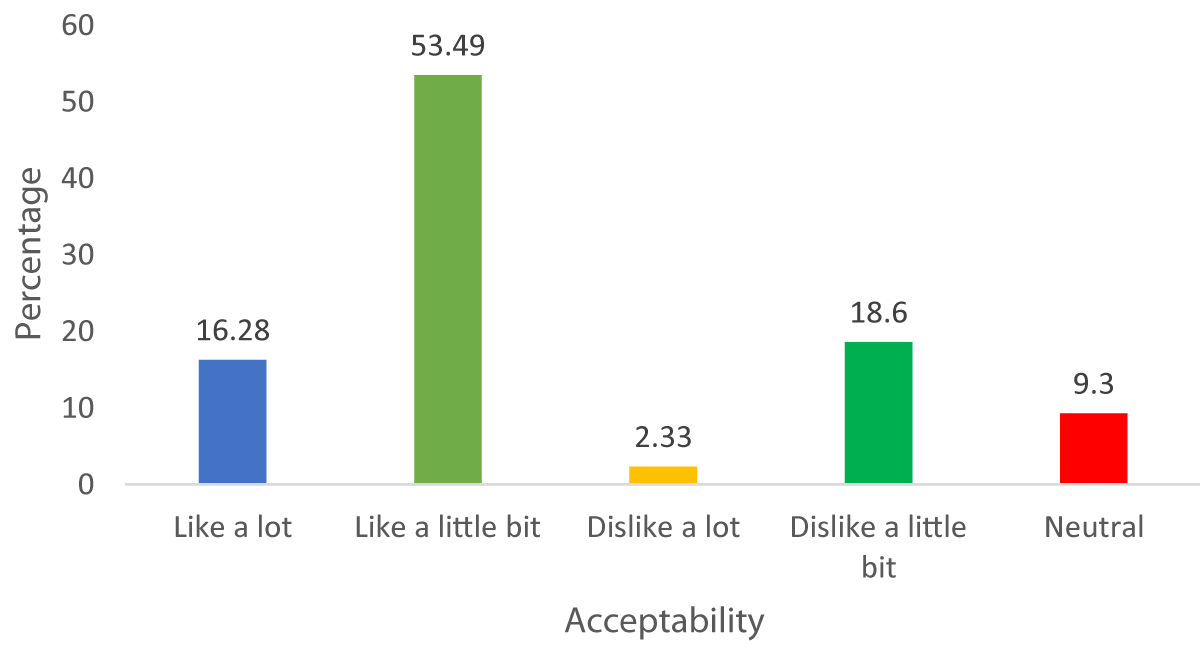
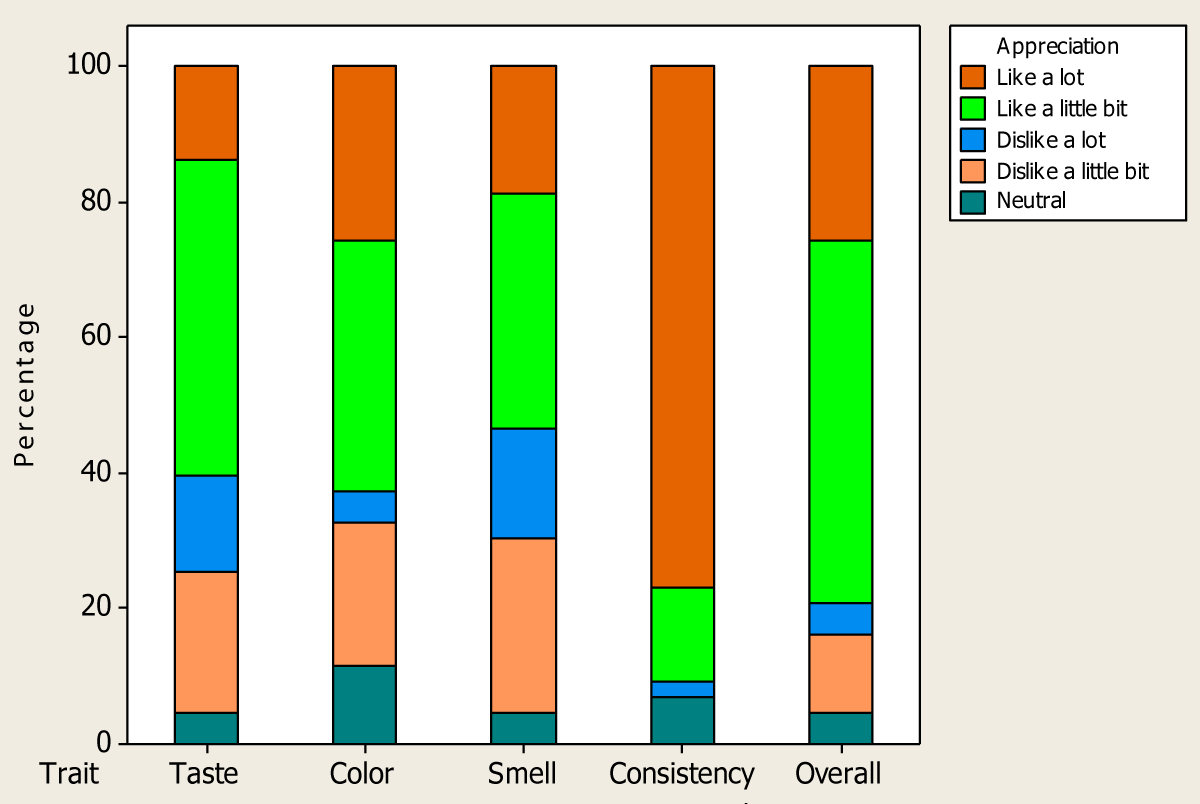
Figures 2,3 present the results of the hedonic test carried out on the children (Figure 2) and their mothers (Figure 3).
Figure 2: Appreciation of the MOL-flour supplement porridge by children.
Figure 3: Mothers’ appreciation of the MOL supplement porridge.
Among the children, 69.77% liked the porridge (with a minimum score of 4), and 9.30% were indifferent. The mothers generally liked the MOL-flour-based porridge in terms of consistency (90%), color (65%), taste (60%), and smell (55%) (with a minimum score of 4).
Prevalence of different types of malnutrition in both groups
In the intervention group, the prevalence of moderate underweightness decreased not significantly by 10.67% from 12% to 1.33% (p > 0.05) (Table 2), while severely acute malnutrition decreased from 8% to 4%.
| Table 2: Prevalence of different types and forms of malnutrition at the beginning and at the end of the study for both the intervention and control groups. | |||||||||
| Start | End | ||||||||
| Good | Moderate | Severe | p | Good | Moderate | Severe | p | ||
| Underweightness (W/A) % | Control (n = 75) | 81.25 | 4.17 | 2.08 | 0.246 | 79.17 | 6.25 | 0.00 | 0.100 |
| Intervention (n = 48) | 72.00 | 12.00 | 0.00 | 92.00 | 1.33 | 0.00 | |||
| Acute Malnutrition (W/H) % | Control (n = 75) | 54.17 | 18.75 | 0.00 | 0.048 | 47.92 | 10.42 | 2.08 | 0.028 |
| Intervention (n = 48) | 33.33 | 21.33 | 8.00 | 50.67 | 6.67 | 4.00 | |||
| Chronic Malnutrition (H/A) % | Control (n = 75) | 37.5 | 22.92 | 10.42 | 0.001 | 31.25 | 29.17 | 8.33 | 0.009 |
| Intervention (n = 48) | 2.67 | 38.67 | 18.67 | 8.00 | 40.00 | 14.67 | |||
| weight-for-Age (W/A); Height-for-Age (H/A) and Weight-for-Height (W/H) | |||||||||
Moreover, another trend was observed with moderately acute malnutrition where the proportion of malnourished children significantly decreased from 21.33% to 6.67% (p ˂ 0.05), and chronic malnutrition which significantly also decreased from 18.67% to 14.67% (p ˂ 0.05).
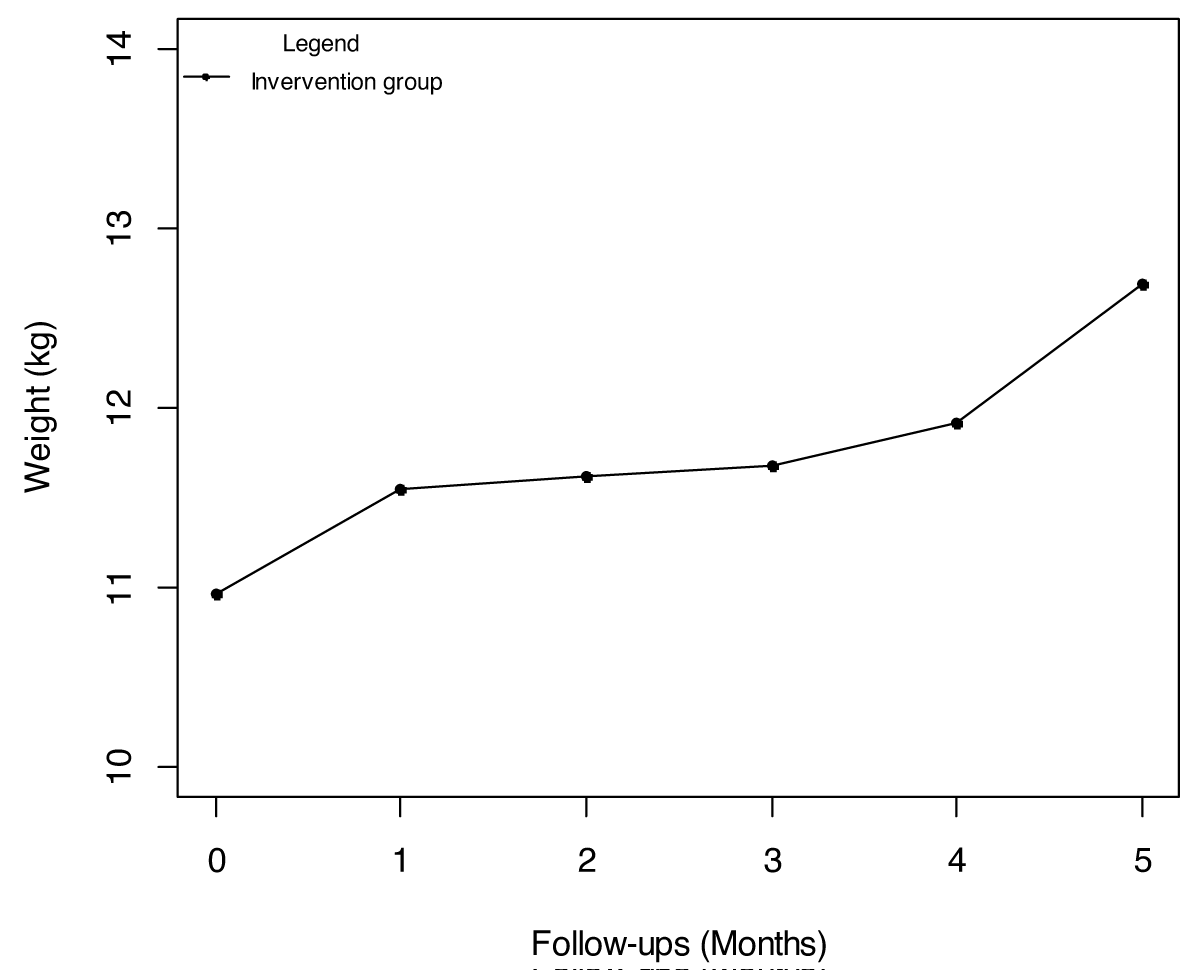
Weight gain in children in both the control and intervention groups
As shown in Table 3, the average weight of children at the beginning of the study was similar in both groups (p > 0.05), namely an average of 10.64 kg in the control group and 10.96 kg in the intervention group. The follow-up in the intervention group showed that the children’s weight changed positively (Figure 4). At the first follow-up, the children’s weight was 11.55 kg, which represents an increase of 586 g from the initial weight. The second, third, fourth, and fifth follow-ups showed increases of 75g, 49g, 246g, and 765g, respectively. The average weight gain by the children in the control group was 1.08 kg which is significantly lower than those in the intervention group, which was 1.72 kg (p ˂ 0.05).
| Table 3: Average weight gain by children in the control and intervention groups. | ||||
| Parameter | Control (n = 75) |
Intervention (n = 48) |
p - value | |
| Weight (kg) | Start (T0) | 10.64 ± 0.38a | 10.96 ± 0.29a | 0.579 |
| End (T1) | 11.72 ± 0.36a | 12.68 ± 0.30a | 0.069 | |
| Weight Gain (kg) | 1.08 ± 0.14a | 1.72 ± 0.17b | 0.000 | |
| Values that are followed by the same letter on the same line are not significantly different at the 5% level. | ||||
Figure 4: Changes in the children’s weight in the intervention group.
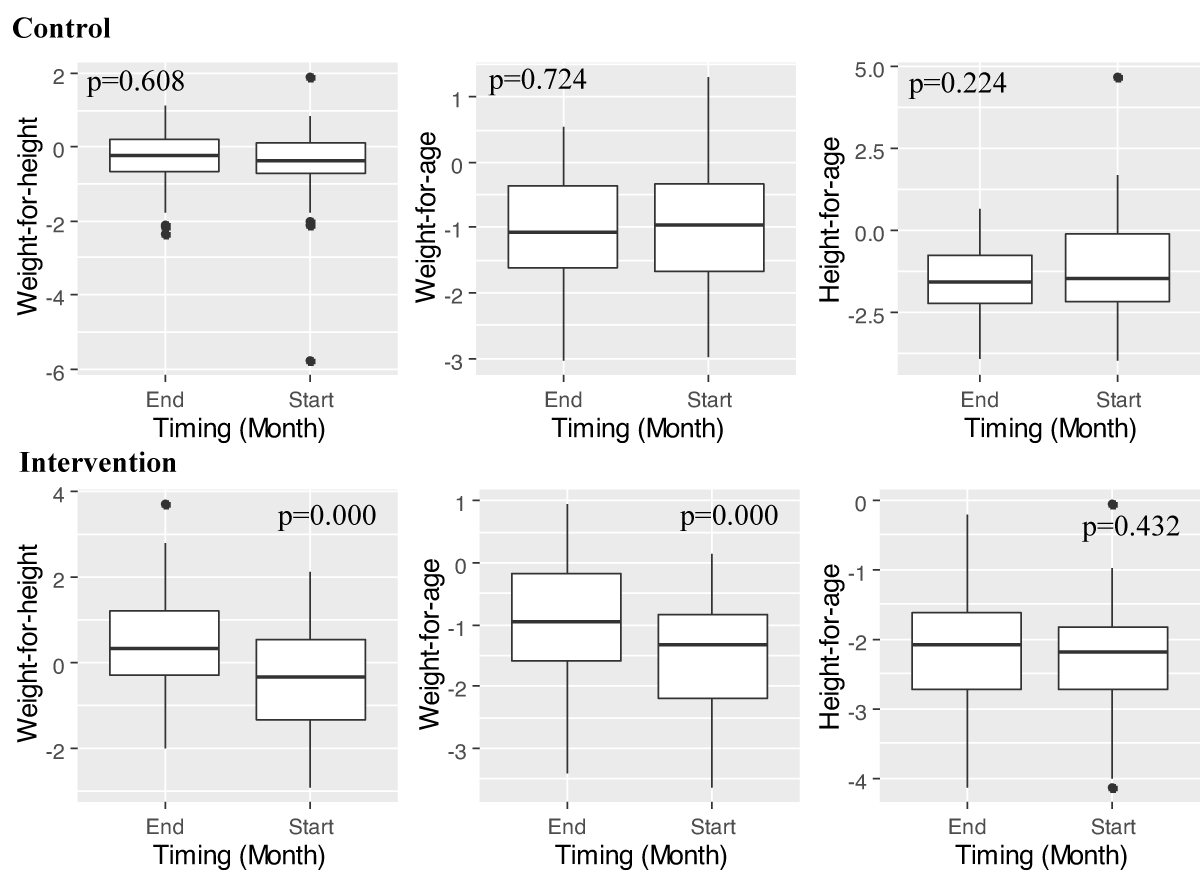
Changes in z-scores
Figure 5 shows the evolution of the z-scores of the anthropometric indices in the children of the control and intervention groups at the beginning and at the end of the study. For the control group, the mean weight-for-height z-scores at baseline (-0.45) improved not significantly (p > 0.05) by the end of the study (-0.34). The mean weight-for-age z-scores also improved not significantly (p > 0.05). Thus, a mean weight-for-age z-score of -1.08 was recorded at the beginning of the intervention, as opposed to -1.02 at the end of it. Regarding the mean height-for-age z-scores, no significant difference (p > 0.05) was observed between the values recorded at the beginning (-1.56) and at the end (-1.23) of the study.
Figure 5: Changes in weight-for-height, weight-for-age and height-for-age z-scores in children of the control and intervention groups at baseline and at the end of the study. WHZ: Weight-for-Height Z-scores; WAZ: Weight-for-Age Z-scores; HAZ: Height-for-Age Z-scores.
For the intervention group, the mean weight-for-height z-scores at baseline (-0.35) improved significantly (p ˂ 0.05) by the end of the study (0.43). The mean weight-for-age z-scores also improved not significantly (p ˂ 0.05). Thus, a mean weight-for-age z-score of -1.48 was recorded at the beginning of the intervention, as opposed to -0.93 at the end of it. Regarding the mean height-for-age z-scores, no significant difference (p > 0.05) was observed between the values recorded at the beginning (-2.26) and at the end (-2.15) of the study.
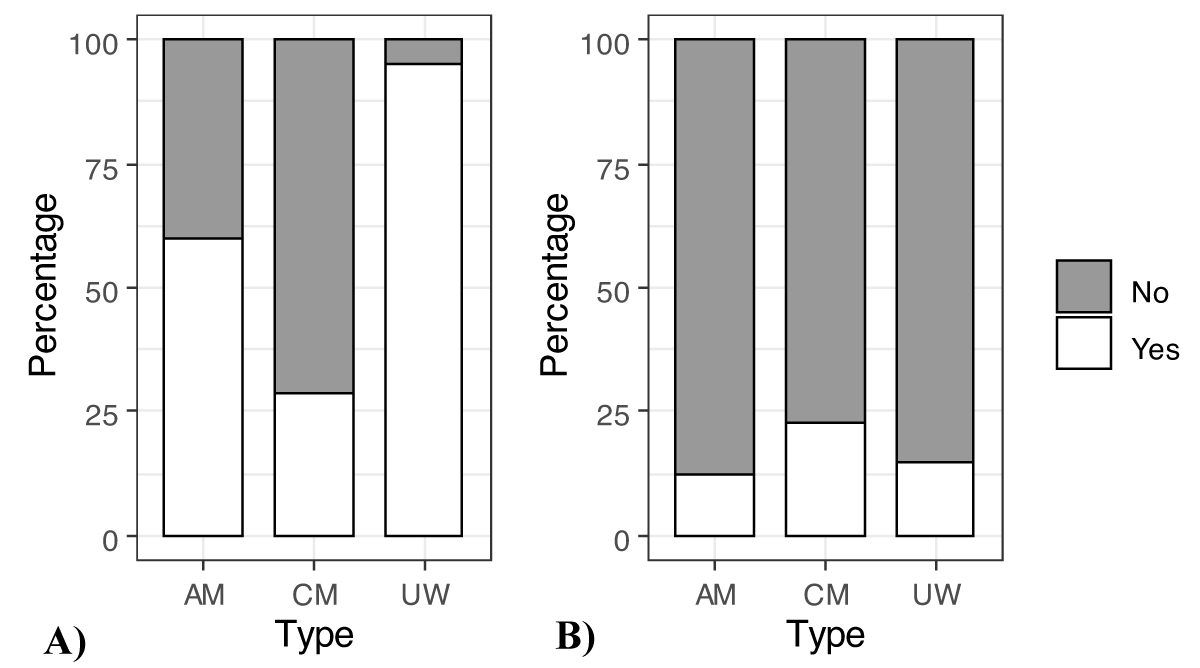
Among the children in the intervention group (B) who were underweight at the start of the study, 95.24% of them left their malnutrition state for a better state (Figure 6) and improvements of 60% (acute malnutrition) and 28.77% (chronic malnutrition) were observed at the end of the study.
Figure 6: Improvement in the prevalence of malnutrition among children in the control and intervention groups. UW: Underweightness; AM: Acute Malnutrition; CM: Chronic Malnutrition. A): Control; B): Intervention.
As for the control group (A), among the children who were underweight at the start of the study, 85.42% of them left their malnutrition state for a better state (Figure 6) and improvements of 12,5% (acute malnutrition) and 22.92% (chronic malnutrition) were observed at the end of the study.
The objective of the present study was to assess the impact of a supplemental porridge with Moringa oleifera leaf (MOL)-flour on the weight of moderately acutely malnourished (MAM) children.
Our results show a significant increase in the weight of malnourished children who have been fed MOL-flour porridge, compared to those who did not consume the porridge. A similar result was found in the study conducted by Zongo, et al. [27], Ndong, et al. Houessou, et al. [24], Tété-Benissan, et al. [26], and Tahiliani, et al. [38]. In Guinea, Shiriki, et al. [11] used four different flour formulations based on corn, soy, peanut; and MOL flour, and the one containing MOL flour gave the best performance, as revealed in tests. By the same token, research conducted by Houndji, et al. (2013) and carried out in Benin, revealed that a daily intake of 10 g of MOL flour improves significantly the nutritional status of children for emaciation, growth retardation, as well as for underweightness. On the other hand, Boateng, et al. [12] highlighted that the addition of a daily dose of 5 g of MOL flour to the usual infant diet for four months, did not significantly improve the children’s growth [25]. This observed result could be due to the different quantities of MOL flour used. In addition, this could be due to the various food mixed together and added to the MOL flour. Based on the Global Food Index [39], the present study used a food matrix made up of corn, malted sorghum, soy, peanut, milk, MOL flour, and salt while Boateng, et al. [12] used just corn, sorghum, and MOL-flour.
We have observed that the use of MOL-flour porridge has significantly contributed to a reduction in the prevalence of malnutrition in children for underweightness, acute, and chronic malnutrition with an average weight gain of 1,720 g at the end of the intervention, and with a significant improvement in the nutritional status of malnourished children. Houndji, et al. [23] have highlighted the same trends of significant improvement in the nutritional status of children for wasting, stunting, and underweightness conditions in Benin, with a daily intake of 10 g of MOL flour [23]. Similarly, a nutritional intervention in India with a daily intake of 30 g of MOL flour for 2 months showed significant improvement in the form of weight gain in children with grades I and II protein energy malnutrition [23].
With regard to chronic malnutrition, the impact of MOL flour is less important. This is potentially due to the health condition or the genetic makeup of the children. Poor health status is often associated with a deterioration of nutritional status [1,40–43]. On the other hand, the pathogenesis of stunting involves changes in deoxyribonucleic acid (DNA) [21]. Health status is also a factor that may influence the nutritional status of children [32]. Indeed, 63% of children experienced illnesses during the study. The occurrence of illnesses (such as diarrhea) in the two weeks prior to the surveys, age, gender, immunization status of the child, education level, mother’s occupation, type of fuel used in the household, and level of expenditure on child nutrition were all factors which significantly influence the z-scores of the said children [44]. The health condition of chronically malnourished children may have prevented nutrient absorption since the consumption of MOL flour can induce changes in DNA sequences in the pathogenesis of stunting through nutri-genomic and bio-molecular mechanisms [32].
Acceptability testing is a necessary step in the development of a new product [45]. Overall, the MOL-flour porridge used as a test food was accepted by 70% of the children and by more than 75% of the mothers. This high percentage of acceptability by both the children and mothers is potentially due to the select raw materials used and to the quality of the formulation, which gave it a good taste, good color, and good consistency with a pleasant smell. This result can be attributed to the selection of local food resources that are already part of the eating habits of the child-mother duo. Similar results of porridge acceptability were obtained by Bello, et al. [9] who evaluated the physicochemical and sensory properties of complementary foods derived from mixtures of sorghum (malted or not), soybean, and MOL-flour at different percentages. They found that the porridge made with malted sorghum and a 10% MOL-flour formulation was the most accepted and had the best scores of sensory attributes.
We have determined that the non-acceptance of the porridge by a few children and mothers is due to the unusual green color of the porridge. This result agrees with the work done by Houndji, et al. [23]. Familiarity with the ingredients involved therefore seems to be an important factor affecting the acceptability of the final product.
The present study has assessed the impact of a supplemental porridge with Moringa oleifera leaf (MOL) flour on the weight gain of malnourished children. At the end of the study, the results have shown that this porridge, globally appreciated by the children and their mothers, has significantly improved the weight gain, weight/height, and weight/age z-scores of children who were fed with the MOL flour (intervention group) as opposed to those who were not so fed (the control group). Overall, MOL-flour-supplemented porridge can be used in the prevention or improvement of weight gain in moderately to mildly malnourished children. Nevertheless, additional research about masking the smell of the MOL flour in the porridge will probably increase its acceptability and, as a result, deliver better results.
The School of Nutrition and Sciences and Technologies, Faculty of Agricultural Sciences, University of Abomey-Calavi, Benin; are acknowledged for their contribution towards this research. This research is supported by the project named FortiMoringa.
- Ngo J, Serra-Majem L. Hunger and Malnutrition. Reference Module in Food Science. 2018.
- The Republic of Mozambique multisectorial plan for chronic malnutrition reduction in Mozambique list of abbreviations and acronyms. 2020; 2014 (July 2010).
- National Institute of Statistics and Economic Analysis (INSAE), World Food Program, Unicef and FAO. Global Analysis of Vulnerability, Food Security and Nutrition (AGVSAN), 2009; 168.
- National Institute of Statistics and Economic Analysis (INSAE) and I. Demographic and Health Survey of Benin 2011-2012. Calverton, Maryland, USA Insa ICF Int. 2013.
- Kennedy GL, CARI, IPC, Derrickson JP, Fisher AG, Anderson JEL. The CARI and the IPC. The Journal of Nutrition. 2015; 18: 1–5. http://dx.doi.org/10.1007/s11027-014-9627-7%0Ahttp://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html%0Ahttp://dx.doi.org/10.1016/j.nut.2009.05.001
- Shaheen R, Streatfield PK, Naved RT, Lindholm L, Persson LA. Equity in adherence to and effect of prenatal food and micronutrient supplementation on child mortality: results from the MINIMat randomized trial, Bangladesh. BMC Public Health. 2014 Jan 7;14:5. doi: 10.1186/1471-2458-14-5. PMID: 24393610; PMCID: PMC3893435.
- Svefors P, Selling KE, Shaheen R, Khan AI, Persson LÅ, Lindholm L. Cost-effectiveness of prenatal food and micronutrient interventions on under-five mortality and stunting: Analysis of data from the MINIMat randomized trial, Bangladesh. PLoS One. 2018 Feb 15;13(2):e0191260. doi: 10.1371/journal.pone.0191260. PMID: 29447176; PMCID: PMC5814099.
- Allen L, De Benoist B, Dary O, Hurrell R. Guidelines on food fortification with micronutrients Food and Agricultural Organization of the United Nations Guidelines on food fortification with micronutrients. 2006; 341. https://www.who.int/nutrition/publications/guide_food_fortification_micronutrients.pdf
- Bello A, Gernah D, Ariahu C. Physico-Chemical and Sensory Properties of Complementary Foods from Blends of Malted and Non-Malted Sorghum, Soybean and Moringa Oleifera Seed Flours. Am J Food Sci Technol. 2020; 8:1–13.
- Black RE, Makrides M, Ong KK. Complementary Feeding: Building the Foundations of Healthy Life. Nestlé Nutrition Institute Workshops Series. Basel, Switzerland, Karger; Vevey, Nestlé: Switzerland. 2017;
- Shiriki D, Igyor M, Gernah D. Nutritional Evaluation of Complementary Food Formulations from Maize, Soybean and Peanut Fortified with Moringa oleifera Leaf Powder. Food Nutr Sci. 2015; 6:494–500.
- Boateng L, Quarpong W, Ohemeng A, Asante M, Steiner-Asiedu M. Effect of complementary foods fortified with Moringa oleifera leaf powder on hemoglobin concentration and growth of infants in the Eastern Region of Ghana. Food Sci Nutr. 2018 Nov 20;7(1):302-311. doi: 10.1002/fsn3.890. PMID: 30680185; PMCID: PMC6341130.
- Awogbenja M, Osundahunsi O, Fagbemi T. Chemical Functional and Sensory Properties of Complementary Diets from Blends of Fermented Millet (Penniselum glaucum) with Groundnut (Arachis hypogeae) and Moringa oleifera Seed Flours. Journal of Family Medicine and Health Care. 2020; (6):97–105.
- Maternal and Child Nutrition Study Group; Group members:; Black RE, Alderman H, Bhutta ZA, Gillespie S, Haddad L, Horton S, Lartey A, Mannar V, Ruel M, Victora CG, Walker SP, Webb P. Maternal and child nutrition: building momentum for impact. Lancet. 2013 Aug 3;382(9890):372-375. doi: 10.1016/S0140-6736(13)60988-5. Epub 2013 Jun 6. PMID: 23746778.
- Kouton S, Hounkpatin W, Ballogou V, Lokonon J, Soumanou M. Characterization of the diet of young children aged 6 to 36 months in rural and urban areas of southern Benin. J Appl Biosci. 2017; 110(1):10831-10840.
- PMASN. Multisectoral Food, Health and Nutrition Project. 2014.
- Haider BA, Bhutta ZA. Multiple-micronutrient supplementation for women during pregnancy. Cochrane Database Syst Rev. 2017 Apr 13;4(4):CD004905. doi: 10.1002/14651858.CD004905.pub5. Update in: Cochrane Database Syst Rev. 2019 Mar 14;3:CD004905. PMID: 28407219; PMCID: PMC6478115.
- Palmese F, Bolondi I, Giannone FA, Zaccherini G, Tufoni M, Baldassarre M, Caraceni P. The Analysis of Food Intake in Patients with Cirrhosis Waiting for Liver Transplantation: A Neglected Step in the Nutritional Assessment. Nutrients. 2019 Oct 15;11(10):2462. doi: 10.3390/nu11102462. PMID: 31618837; PMCID: PMC6836082.
- Srikanth V, Mangala S, Subrahmanyam G. Improvement of Protein Energy Malnutrition by Nutritional Intervention with Moringa Oleifera among Anganwadi Children in Rural Area in Bangalore, India. Int J Sci Study. 2014; 2.
- Dekpemadoha J, Idohou R, Adjadogbedji-Avouzoukan S, Kayode A, Hounhouigan D. Chadaré FJ, Madode YE, Fanou-Fogny N, Ayosso JO, Sacla Aidé E. Nutritional choice guide for local food resources (RAL) in the agro-ecological zones (ZAE) of Benin. Cotonou, Benin. 2017.
- Putra A, Setiawan N, Sanjiwani M. Nutrigenomic and Biomolecular Aspect of Moringa oleifera Leaf Powder as Supplementation for Stunting Children. J Trop Biodivers Biotechnol. 2021; 26.
- Oyeyinka A, Oyeyinka S. Moringa oleifera as a food fortificant: Recent trends and prospects. Review article. J Saudi Soc Agric Sci. 2018; 17: 127-136.
- Houndji S, Bodjrenou F, Londji S. Improvement of the nutritional status of children aged 6 to 30 months in Lissèzoun (Centre-Benin) using Moringa oleifera leaf powder (Lam.). Int J Biol Chem Sci. 2013; (7):225–35.
- Houessou A. Formulation and characterization of infant flours enriched with Moringa oleifera leaf powder: optimization of the nutritional and microbiological value and evaluation of the sensory attributes of the products. MSc, University of Abomey-calavi. 2018; 43.
- Ndong M, Wade S, Dossou N, Diagne R. Nutritional value of Moringa oleifera, study of iron bioavailability, effect of enriching various traditional Senegalese dishes with leaf powder. Developing African leafy vegetables for improved nutrition. 2005;
- Tété-Bénissan A, Quashie M, Lawson-Evi K, Kokou K, Gbeassor M. Nutritional recovery in HIV-positive and HIV-negative malnourished subjects after using Moringa oleifera Lam. leaves. J Anim &Plant Sci. 2012; 15(2):2184-99.
- Zongo U, Zoungrana S, Savadogo A, Traoré A. Nutritional and clinical rehabilitation of severely malnourished children with Moringa oleifera Lam. leaf powder in Ouagadougou (Burkina Faso). Food Nutr Sci. 2013; 4(09):991.
- Gopalakrishnan L, Doriyaa K, Kumara D. Moringa oleifera: A review on nutritive importance and its medicinal application. Food Science and Human Wellness. 2016;(5):49–56.
- Agossadou J, Chadare F, Nago E. Effect of consumption of foods fortified with baobab fruit pulp and moringa leaf powder on the nutritional status of children. Ruforum Work Doc Ser. 2016; 14:979–88.
- Adetola O, Onabanjo O, Stark A. The search for sustainable solutions: Producing a sweet potato-based complementary food rich in vitamin A, zinc, and iron for infants in developing countries Scientific African. 2020;8.
- PAM. Global Analysis of Vulnerability, Food Security and Nutrition (AGVSA) in Benin. 2017;
- ICF National Institute of Statistics and Economic Analysis (INSAE) and Demographic and Health Survey in Benin, 2017-2018. Cotonou, Bénin Rockville, Maryland, USA Insa ICF. 2019;
- Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009 Nov;41(4):1149-60. doi: 10.3758/BRM.41.4.1149. PMID: 19897823.
- Balkin R, Sheperis C. Evaluating and Reporting Statistical Power in Counseling Research. Journal of Counseling & Development. 2011; 89.
- Madrelle J, Lange C, Boutrolle I, Valade O, Weenen H, Monnery-Patris S, Issanchou S, Nicklaus S. Development of a new in-home testing method to assess infant food liking. Appetite. 2017 Jun 1;113:274-283. doi: 10.1016/j.appet.2017.03.002. Epub 2017 Mar 6. PMID: 28274649.
- OMS. Training course on child growth assessment. WHO Child Growth Standards. Facilitator's Manual. 2008;
- Child Growth Standards : World Health Organization/Nutrition for Health and Development/Sustainable Development and Healthy Environmental. Organ Mond la Santé, Washington, DC. 2006;
- Tahiliani P, Kar A. Role of Moringa oleifera leaf extract in the regulation of thyroid hormone status in adult male and female rats. Pharmacol Res. 2000 Mar;41(3):319-23. doi: 10.1006/phrs.1999.0587. PMID: 10675284.
- Development and evaluation of the quality of an infant flour supplement with high nutritional density from local food resources. Thesis for obtaining the Master's degree in agronomic sciences, option Sciences and Technology. 2016;
- Drake LJ, Lazrak N, Fernandes M, Chu K, Singh S, Ryckembusch D, Nourozi S, Bundy DAP, Burbano C. Establishing Global School Feeding Program Targets: How Many Poor Children Globally Should Be Prioritized, and What Would Be the Cost of Implementation? Front Public Health. 2020 Dec 2;8:530176. doi: 10.3389/fpubh.2020.530176. PMID: 33344395; PMCID: PMC7738473.
- Darnton-Hill I, Mkparu UC. Micronutrients in pregnancy in low- and middle-income countries. Nutrients. 2015 Mar 10;7(3):1744-68. doi: 10.3390/nu7031744. PMID: 25763532; PMCID: PMC4377879.
- Harika R, Faber M, Samuel F, Kimiywe J, Mulugeta A, Eilander A. Micronutrient Status and Dietary Intake of Iron, Vitamin A, Iodine, Folate and Zinc in Women of Reproductive Age and Pregnant Women in Ethiopia, Kenya, Nigeria and South Africa: A Systematic Review of Data from 2005 to 2015. Nutrients. 2017 Oct 5;9(10):1096. doi: 10.3390/nu9101096. PMID: 28981457; PMCID: PMC5691713.
- Phillips EA, Comeau DL, Pisa PT, Stein AD, Norris SA. Perceptions of diet, physical activity, and obesity-related health among black daughter-mother pairs in Soweto, South Africa: a qualitative study. BMC Public Health. 2016 Aug 9;16:750. doi: 10.1186/s12889-016-3436-8. PMID: 27506678; PMCID: PMC4977727.
- Razafindrazaka R. Development and evaluation of a strategy to improve complementary feeding of young children in Brickaville (East Coast of Madagascar). Doctoral thesis, University of Antananarivo, Antananarivo, Madagascar. 2006;
- Torrico D, Sharma C, Dong W. Virtual reality environments on the sensory acceptability and emotional responses of no- and full-sugar chocolate. LWT-.Food Sci Technol. 2020.