More Information
Submitted: October 30, 2023 | Approved: November 11, 2023 | Published: November 13, 2023
How to cite this article: Osuka Y, Masutomi H, Nakamura S, Tanigawa C, Ishihara K, et al. Improvements in the Subjective Sleep of Japanese Middle-aged Managers from the Consumption of an Edible Film Containing Crocetin. Arch Food Nutr Sci. 2023; 7: 088-096.
DOI: 10.29328/journal.afns.1001054
Copyright License: © 2023 Osuka Y, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Crocetin; OSA-MA; InSomnograf®; Sleep quality; Frequent dreaming
Improvements in the Subjective Sleep of Japanese Middle-aged Managers from the Consumption of an Edible Film Containing Crocetin
Yusuke Osuka1#, Hirofumi Masutomi1#*, Shuji Nakamura2, Chiemi Tanigawa2, Katsuyuki Ishihara1, Masashi Yanagisawa2,3 and Toshio Kokubo2,3
1#Research & Development Division, Calbee Inc, Utsunomiya, Tochigi 321-3231, Japan
2#S’UIMIN Inc., Shibuya-ku, Tokyo 151-0061, Japan
3#International Institute for Integrative Sleep Medicine (WPI-IIIS), University of Tsukuba, Tsukuba, Ibaraki 305-8575, Japan
#Equal contribution
*Address for Correspondence: Hirofumi Masutomi, Research & Development Division, Calbee Inc, 23-6, Kiyohara-kogyodanchi, Utsunomiya, Tochigi 321-3231, Japan, Email: [email protected]
It has been reported that Japanese people sleep for an average of 7 hours and 22 minutes per night, with those in their 40s and 50s sleeping the least. This is much less than in other developed countries. Aging has also been reported to decrease the total sleep time and sleep latency as well as increase wake after sleep onset (WASO). Crocetin is a carotenoid with antioxidant activity. It has been reported that 14 consecutive days of crocetin intake increases delta power during sleep and decreases WASO. However, the benefits of short-term ingestion have not been clarified. In this double-blind, randomized crossover study, we examined the effects of crocetin-containing edible films consumed for seven consecutive days on the sleep quality of healthy Japanese subjects working in management positions who were aged 45 years or older.
The study participants comprised 20 subjects (12 males and 8 females; mean age 50.4 ± 4.8 years; body mass index (BMI) 22.5 ± 2.7). An electroencephalography (EEG) measuring device (InSomnograf®) was used to measure sleep objectively and a questionnaire, OSA Sleep Questionnaire MA version (OSA-MA) was used to assess sleep subjectively upon waking. The crocetin group demonstrated significantly higher values of OSA-MA Factor 3 (frequent dreaming) than the placebo group (placebo: 46.8 ± 6.9; crocetin: 49.5 ± 7.4). No differences were observed for the other four factors. No differences were observed in the sleep parameters determined with InSomnograf®.
Our findings suggest a new effect of crocetin on sleep quality of frequent dreaming.
It has been reported that as many as one in five Japanese people (and one in three people over 60 years old) currently suffer from a sleep disorder [1,2]. It has been epidemiologically proven that sleep disorders and the resulting sleep debt are closely related to mood disorders, metabolic syndromes, dementia, and even cancer [3-6]. According to the Gender Data Portal (2021) of the Organization for Economic Cooperation and Development (OECD), the average sleep duration of Japanese people is 7 hours 22 minutes, the lowest among member countries [7]. Japanese people in their 40s and 50s sleep the least; 58% of those in their 40s and 79% of those in their 50s slept fewer than 7 hours, according to the Ministry of Health, Labor and Welfare's 2021 Health Status Survey report [8]. Various types of sleep problems have also been reported, with 12% of those in their 40s and 50s reporting difficulties falling asleep, 16% reporting frequent wake after sleep onset (WASO), 14% reporting early awakenings, 12% reporting dissatisfaction with their sleep quality, and 18% reporting excessive daytime sleepiness. Only 9% of respondents had no problems [8].
Age-related changes to sleep patterns are widely known and have been demonstrated to decrease the total sleep time, prolong the sleep latency, fragment sleep (e.g., an increased number of WASO), increase the proportion of non-REM in sleep stages N₁ and N₂, and decrease the proportion of REM and non-REM in sleep stage N₃ [9]. These changes gradually decline as the basal metabolism declines and, with the exception of the prolonged sleep latency, are said to plateau around the age of 60 [10]. The total sleep time has been demonstrated to decrease by an average of 10–12 minutes every 10 years of age. The WASO time has been demonstrated to increase by an average of 9.7 minutes every 10 years of age [10,11]. The prolonged sleep latency does not change significantly between the ages of 30 and 50, whereas it inclines significantly after the age of 50 [12]. Sleep efficiency is reported to decrease by 2.1% with every 10 years of age, with a particularly marked drop from 91.4 ± 4.2% to 80.6% ± 7.9% between the 50s and 60s [11,13].
According to the 2021 Basic Survey on Wage Structure conducted by the Ministry of Health, Labour and Welfare of Japan, the average age of managers is 47 for section managers and 49–52 for department heads, with no significant difference between the sexes [14]. A study on the male employees of a Japanese electrical equipment manufacturing company in the 1990s, which was based on a subjective assessment, observed that workers in their 50s had significantly worse WASO and early awakenings than workers in their 20s to 40s. No sleep problems specific to managers were identified [15]. Promotions to management positions have been reported to temporarily worsen mental health [16]. In a Pittsburgh Sleep Questionnaire Index (PSQI) survey of public employees, the percentage of employees with a total PSQI score of 5.5 or higher was lowest in managerial positions (section chiefs and above) and increased with a move down through the ranks of middle management (assistant section chiefs, section chiefs, etc.) and general positions [17]. Only a few subjective studies have focused on the sleeping status and habits of Japanese managers, and objective studies of sleep, especially for managers, are largely unknown.
Crocetin is a carotenoid compound of the Gardenia genus used in traditional Chinese medicine and as a natural colorant. It is a pharmacologically active substance [18]. Crocetin is known to have a strong antioxidant activity. In a randomized, double-blind crossover study of crocetin intake in healthy adult men with mild sleep disturbances, the number of WASO decreased after 14 consecutive days of crocetin intake, as measured by sleep monitoring with actigraphy [18]. In another randomized, double-blind crossover study of healthy adults with mild sleep complaints, 14 consecutive days of crocetin significantly increased the delta power during sleep, as measured by single-channel electroencephalography [19]. These studies revealed that crocetin intake could improve sleep quality. However, crocetin was administered for 14 consecutive days in these studies; the short-term benefit has not been clear. The subjects were also normal subjects with mild sleep disturbances, and the benefit to normal subjects who do not complain about sleep has not been clarified.
In this study, we investigated the effects of the ingestion of an edible film containing crocetin for seven consecutive days on the sleep of healthy Japanese adult males and females aged between 45 and 70 who were under the stress of Japanese middle-aged managers. To clarify the effects of the ingestion of an edible film containing crocetin for seven consecutive days on sleep, we objectively measured sleep by analyzing the bioelectrical potentials including EEG and subjectively evaluated sleep using questionnaires at bedtime and upon waking.
Study design
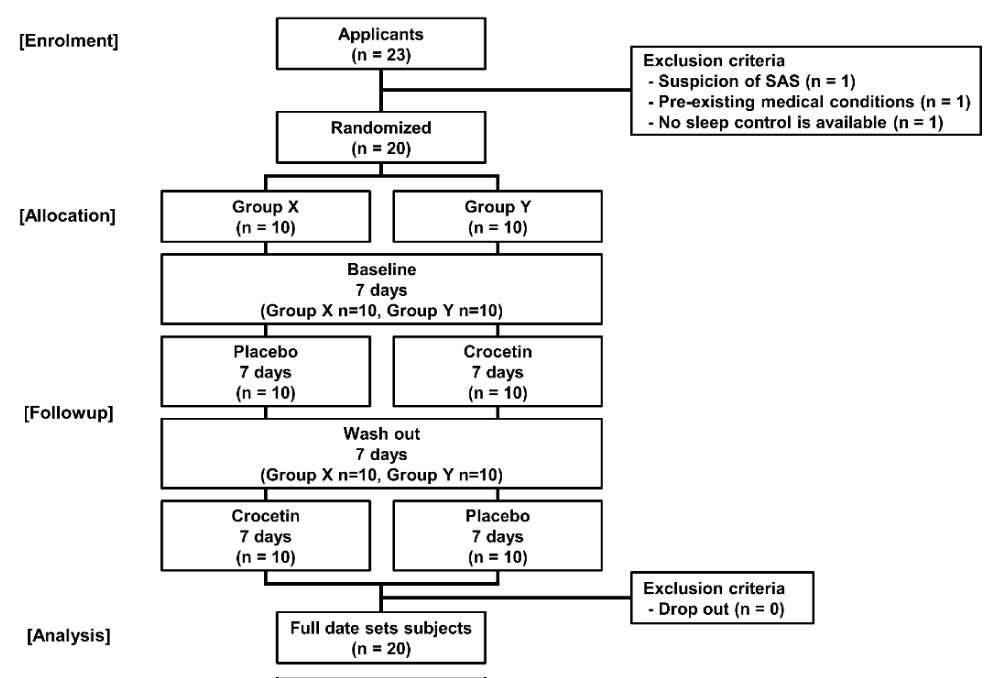
This study was an exploratory, placebo-controlled, randomized, double-blind crossover study. A total of 20 study participants were enrolled using embedded enrollment and the subjects were assigned into two groups (Group X and Group Y) (Figure 1). The subjects were assigned by S.F. in the International Institute for Integrative Sleep Medicine, University of Tsukuba, which was unrelated to the study. Key introductions were performed after the analysis was completed. The study was conducted on selected subjects, according to the research schedule (Table 1). Selected subjects were asked to perform a mild sleep control (sleeping within 2 hours before or after their habitual bedtime and waking
within 2 hours before or after their habitual waking time) from day 1 (Saturday) of the study until the completion of the study. The control was verified using a sleep diary. As a baseline, an objective evaluation of sleep was conducted by measuring electroencephalography (EEG) and other bioelectrical potentials from bedtime to waking time from day 3 to day 7 (Monday to Friday). A questionnaire was administered at bedtime to determine whether there were any behaviors that affected sleep significantly, and another (OSA-MA) upon waking to evaluate sleep subjectively. Group X (10 subjects) received 7 days of a placebo edible film immediately before bedtime in intervention 1 (days 8–14), followed by a 7-day washout period (days 15–21); an edible film containing 7.5 mg crocetin was then administered for 7 days immediately before bedtime in intervention 2 (days 22–28). Group Y (10 subjects) received 7 days of an edible film containing 7.5 mg crocetin immediately before bedtime in intervention 1 (days 8–14), followed by a 7-day washout period (days 15–21); a placebo edible film was then administered for 7 days immediately before bedtime in intervention 2 (days 22–28). Sleep was objectively evaluated by measuring EEG and other bioelectrical potentials from bedtime to waking time for 5 days during the two intake periods (days 10–14 and 24–28 (Monday through Friday)) and subjectively evaluated using the questionnaires (the bedtime questionnaire and OSA-MA) administered at bedtime and upon waking. The test food of edible film containing 7.5 mg crocetin and other ingredients including pullulan, gardenia pigment, glycerin, microcrystalline cellulose, sweeteners (xylitol, aspartame, L-phenylalanine compound, acesulfame K), flavorings, and glycerin fatty acid esters. The placebo films were prepared in such a way that they did not differ in nutritional composition from the test food and were not distinguishable by color, odor, or flavor. These test foods were produced by Tsukioka Film Pharma Co. Ltd. (Gifu, Japan).
Ethical considerations and study protocol registration
This study was conducted in compliance with the Ethical Guidelines for Life Sciences and Medical Research Involving Human Subjects, the Declaration of Helsinki, and the regulations of each medical institution. This study was ethically reviewed by the Ethics Committee of the Chiyoda Para Medical Care Clinic (approval date: August 19, 2022; approval number: 22081906). After the ethical review was completed, the protocol of this study was registered in the University Hospital Medical Information Network Center Clinical Trial Registration (UMIN-CTR) system (registration number: UMIN000048733).
Subject selection
Subjects were recruited from Calbee Inc. if they met the following recruitment criteria: they were aged between 45 and 70 years old, worked as managerial staff (section manager or above), and consented to participate.
The exclusion criteria were as follows: those who were taking any medication, or who may have been required to take medication (e.g., antiallergic drugs, sleep aids, etc.) that could have affected the study, for one month prior to the start of the consumption of the test food and during the study period; those who regularly used specific health foods, functional foods, supplements, or other foods more than three times a week that could have affected the study, including those who were unable to limit their intake during the study period; those with a history or current experience of serious diseases of the heart, liver, kidneys, digestive organs, etc.; those with suspected chronic or acute serious infectious diseases; those scheduled for a vaccination during the study period; those who were pregnant or planning to become pregnant, or who were breastfeeding; those who habitually drank alcohol more than three times a week and more than 180 mL sake or equivalent (beer: 500 mL; whiskey: 60 mL; shochu (Japanese liquor similar to vodka): 108 mL); those with extremely irregular eating habits; those with a body mass index (BMI) of 30 or greater; those planning significant lifestyle changes during the study period; those whose sleep may have been disturbed by external factors (e.g., family members or pets); those who were allergic to the test food; those who were currently participating in clinical research on other drugs or health foods, or who were scheduled to participate in other clinical research programs within one month after the completion of the research or after consenting to participate in such research; and those who were judged to be inappropriate for participation in this study by the principal investigator.
K6 questionnaires (K6)
K6 is a questionnaire that was developed by R C Kessler, et al. with support from the U.S. government's National Center for Health Statistics in the National Health Interview Survey (NHIS) [20]. Its equivalence in a Japanese version has been confirmed and is primarily used for mental health screening purposes [21]. The questionnaire asks respondents to answer six questions regarding psychological stress (depression and anxiety) occurring in the past 30 days using a 5-point method. Each question receives a score from 0 to 4. Of a total of 24 points, 5 or more points are equivalent to a psychological stress reaction, 9 or more points are equivalent to a mood/anxiety disorder, and 13 or more points are equivalent to a severe mental disorder [21]. We administered this questionnaire approximately one month prior to the start of the study to determine the daily psychological stress state of our subjects and collected the responses.
Epworth Sleepiness Scale (ESS)
The Epworth Sleepiness Scale (ESS) is a self-assessment method developed by M W Johns for excessive daytime sleepiness. The Japanese version has been verified for authenticity and validity [22,23]. Respondents are asked to choose from four options in eight situations. Each question is assigned a score from 0 to 3. Of a total of 24 points, a score of 5 or greater indicates mild daytime sleepiness and a score of 11 or greater indicates excessive daytime sleepiness. This assessment was administered approximately one month prior to the start of our study to determine the daytime sleepiness of the subjects and to exclude potential suffering from obstructive sleep apnea syndrome.
Athens Insomnia Scale (AIS)
The Athens Insomnia Scale (AIS) is a universal self-assessment instrument for insomnia that was developed by the World Project on Sleep and Health, led by the World Health Organization (WHO). It was later validated for its authenticity and validity [24,25]. The AIS consists of eight questions (sleep onset, WASO, final awakenings, total sleep time, sleep quality, well-being, functional capacity, and daytime sleepiness). The survey asks respondents to select from a choice of four options those that have been experienced at least three times in the past month. Each question is assigned a score of 0~3. Of a total of 24 points, a score of 4 or greater is considered to be indicative of insomnia, and a score of 6 or greater is considered to be highly likely to be insomnia. To ascertain whether or not the subjects in our study had a tendency towards insomnia, we administered the survey approximately one month prior to the start of the study.
Sleep diary/bedtime questionnaire
Sleep diaries were produced in an open-ended format and included the following items: bedtime, time of sleep onset, time and duration of WASO, time of last awakening, time one gets up, and sleep duration. The survey was administered every morning from day 1 to day 28 to determine the bedtime and waking time of each subject. The subjects completed the questionnaire immediately after waking up.
The bedtime questionnaire was a multiple-choice instrument that included the following items: presence or absence of daytime sleepiness or fatigue, presence or absence of naps, duration of naps, presence or absence of exercise longer than 30 minutes, start time of the exercise, presence or absence and frequency of going out, duration of going out, means of transportation when going out, whether or not participants had dinner, start time of dinner, time required for dinner, presence or absence of alcohol consumption, caffeine consumption before or after dinner, whether or not participants had baths, whether or not participants required sleep aids or insomnia medication, and whether or not participants consumed cold remedies that rendered them drowsy. A total of 15 days were administered (day 3 to day 7, day 10 to day 14, and day 24 to day 28) to determine whether or not the behaviors of the subjects affected their sleep (Table 1). The subjects completed this questionnaire approximately 15 minutes before bedtime.
Sleep electroencephalography (InSomnograf®)
S'UIMIN's portable EEG device, InSomnograf® is equipment that measures the bioelectrical potentials including EEG, electromyography (EMG), and electrooculography (EOG) with 5 electrodes, and the sleep stage of each 30 seconds (epoch) during sleep is determined according to AASM scoring manual. It has an 86.9% correlation with polysomnography (PSG) [26]. Parameters related to sleep quality and quantity, which were calculated from the results of the sleep staging (hypnogram), were used in the analysis. These were light-off time, light-on time, total recording time, time of sleep onset, time of last awakening, median sleep time, time spent lying down after last awakening, sleep latency, REM sleep latency, not-scored total time, N1 total time, N1 occurrence rate (%), N2 total time, N2 occurrence rate (%), N3 total time, N3 occurrence rate (%), REM sleep total time, REM sleep occurrence rate (%), total sleep time, WASO total time, and sleep efficiency (%). A total of 15 days were administered (day 3 to day 7, day 10 to day 14, and day 24 to day 28) to determine the sleep parameters of the subjects (Table 1). The subjects wore the device immediately before bedtime to conduct the EEG measurements.
Oguri-Shirakawa-Azumi sleep inventory MA version (OSA-MA)
The Oguri–Shirakawa–Azumi sleep inventory MA version (OSA-MA) is a questionnaire that assesses subjective sleep quality during waking hours for middle-aged and older adults who do not have sufficient time to complete the form or who do not respond appropriately to items with many choices [27]. The questionnaire consists of 16 items covering 5 factors. These are Factor 1 (sleepiness on rising), Factor 2 (initiation and maintenance of sleep), Factor 3 (frequent dreaming), Factor 4 (refreshing), and Factor 5 (sleep length). The OSA Sleep Questionnaire MA version has been subjected to standardization procedures and is sufficiently reliable and reproducible. It was administered for a total of 15 days (day 3 to day 7, day 10 to day 14, and day 24 to day 28) to allow subjects to subjectively assess their sleep (Table 1). Subjects recorded their responses immediately upon waking.
Statistical analysis
GraphPad Prism 8, version 8.4 was used for the statistical analysis. Unpaired t-tests were used for the subject characteristics; Mann–Whitney U tests were used for the K6, ESS, and AIS pre-questionnaires. One-way repeated ANOVA with post hoc Bonferroni tests was used for the analyses of the sleep parameters and OSA-MA. The significance level was set at less than 5%.
Subject screening and pre-survey
In total, 23 individuals volunteered to participate in the study. Three were excluded due to suspected sleep apnea syndrome (SAS), a pre-existing medical history, and difficulty in sleep control (Figure 1). After screening, 20 subjects (12 males and 8 females; mean age 50.4 ± 4.8 years; BMI 22.5 ± 2.7) were randomly assigned into two groups (Table 2). In the pre-test questionnaire, the K6 score indicating depression was 3.1 ± 2.2; the Epworth Sleepiness Scale score, a self-reported method to assess daytime sleepiness, was 10.1 ± 3.6; and the Athens Insomnia Scale, which determines the tendency toward insomnia, was 5.0 ± 3.1. All 20 participants completed the study (Table 3).
Figure 1: Study design. Randomization and screening of subjects. SAS: Sleep Apnea Syndrome.
| Table 1: Study schedule. | |||||||||||||||
| Baseline | Intervention 1 | ||||||||||||||
| Days | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
| Day of the week | Sa. | Su. | Mo. | Tu. | We. | Th. | Fr. | Sa. | Su. | Mo. | Tu. | We. | Th. | Fr. | |
| Sleep control | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | |
| Sleep electroencephalography | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | |||||
| OSA-MA | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | |||||
| Group X | Placebo | ○ | ○ | ○ | ○ | ○ | ○ | ○ | |||||||
| Crocetin | |||||||||||||||
| Group Y | Placebo | ||||||||||||||
| Crocetin | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ||||||||
| Wash out | Intervention 2 | ||||||||||||||
| Days | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 | 28 | |
| Day of the week | Sa. | Su. | Mo. | Tu. | We. | Th. | Fr. | Sa. | Su. | Mo. | Tu. | We. | Th. | Fr. | |
| Sleep control | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | |
| Sleep electroencephalography | ○ | ○ | ○ | ○ | ○ | ||||||||||
| OSA-MA | ○ | ○ | ○ | ○ | ○ | ||||||||||
| Group X | Placebo | ||||||||||||||
| Crocetin | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ||||||||
| Group Y | Placebo | ○ | ○ | ○ | ○ | ○ | ○ | ○ | |||||||
| Crocetin | |||||||||||||||
| OSA-MA: Oguri-Shirakawa-Azumi sleep inventory MA version | |||||||||||||||
| Table 2: Characteristics of subjects. | ||||
| All subjects | Group X | Group Y | p value | |
| N | 20 (12M, 8F) | 10 (5M,5F) | 10 (7M,3F) | |
| Age (year) | 50.4 ± 4.8 | 52.3 ± 4.3 | 48.4 ± 4.7 | 0.071 |
| Height (cm) | 168.2 ± 9.2 | 168.5 ± 10.3 | 167.9 ± 8.5 | 0.889 |
| Weight (kg) | 64.2 ± 13.1 | 63.6 ± 12.1 | 64.8 ± 14.6 | 0.844 |
| BMI (kg/m2) | 22.5 ± 2.7 | 22.2 ± 2.1 | 22.7 ± 3.2 | 0.669 |
| Values are means ± standard deviations (SD). Statistics vs. Group by T-test. BMI; is body mass index. | ||||
| Table 3: Results of a preliminary questionnaire for subjects. | ||||
| All subjects | Group X | Group Y | p value | |
| K6 (score) | 3.1 ± 2.2 | 3.7 ± 2.1 | 2.4 ± 2.3 | 0.216 |
| ESS (score) | 10.1 ± 3.6 | 10.9 ± 3.7 | 9.2 ± 3.6 | 0.322 |
| AIS (score) | 5.0 ± 3.1 | 5.8 ± 3.3 | 4.2 ± 2.9 | 0.264 |
| Values are means ± SD, n = 20. Statistics vs. Group by Mann-Whitney U test. K6: Kessler Psychological Distress Scale; ESS: Epworth Sleepiness Scale; AIS: Athens Insomnia Scale. | ||||
Subjective sleep assessment
The OSA-MA sleep survey resulted in a response rate of 99.3% (298/300). In Factor 3 (frequent dreaming), the crocetin group demonstrated a significant improvement compared with the placebo group (placebo: 46.8 ± 6.9; crocetin: 49.5 ± 7.4) (Table 4). There were no differences in Factors 1 (sleepiness on rising), 2 (initiation and maintenance of sleep), 4 (refreshing), and 5 (sleep length).
| Table 4: Results of OSA-MA scores. | |||
| Baseline | Placebo | Crocetin | |
| OSA1 (Sleepiness on rising) | 42.4 ± 8.3 | 44.9 ± 8.4 | 44.4 ± 8.3 |
| OSA2 (Intention and maintenance of sleep) | 43.6 ± 7.4 | 45.1 ± 6.4 | 46.1 ± 7.4 |
| OSA3 (Frequent dreaming) | 49.8 ± 7.1 | 46.8 ± 6.9 | 49.5 ± 7.4 * |
| OSA4 (Refreshing) | 44.2 ± 8.1 | 45.5 ± 7.8 | 45.4 ± 7.6 |
| OSA5 (Sleep length) | 41.7 ± 8.5 | 43.8 ± 6.6 | 42.9 ± 7.8 |
| OSA total score | 221.2 ± 29.4 | 225.8 ± 22.4 | 228.1 ± 26.8 |
| Values are means ± SD. Statistics vs. Placebo film by way of repeated ANOVA host hoc bonferroni test, *p < 0.05. OSA-MA: Oguri-Shirakawa-Azumi sleep inventory MA version. | |||
Sleep electroencephalography
The rate of compliance for sleep electroencephalography measurements was 93.6% (281/300). None of the parameters related to sleep quality and quantity including total sleep time, sleep efficiency, median sleep time, time of last awakening, time spent lying down after last awakening, time of WASO, total time and occurrence rate of N3, total time and occurrence rate of REM sleep, sleep latency, a number of awakening responses, and REM sleep latency differed between the crocetin and placebo groups (Table 5).
| Table 5: Results of sleep measurement by InSomnograf®. | |||
| Baseline | Placebo | Crocetin | |
| Time in bed (min: sec) | 386:22 ± 34:53 | 373:35 ± 50:41 | 378:04 ± 38:46 |
| Total sleep time (min: sec) | 353:58 ± 32:02 | 343:20 ± 47:44 | 348:28 ± 34:54 |
| Sleep latency (min: sec) | 07:29 ± 04:34 | 07:46 ± 05:34 | 08:17 ± 04:14 |
| Wake After Sleep Onset (min: sec) | 24:49 ± 13:29 | 22:29 ± 10:25 | 21:52 ± 08:45 |
| Non-REM Stage 1 (min : sec) | 18:42 ± 12:29 | 17:59 ± 13:38 | 18:26 ± 14:28 |
| Non REM Stage 2 (min : sec) | 189:38 ± 24:53 | 183:39 ± 37:21 | 183:32 ± 32:00 |
| Non REM Stage 3 (min : sec) | 48:51 ± 23:58 | 49:41 ± 28:19 | 47:04 ± 27:50 |
| REM (min : sec) | 93:33 ± 13:36 | 89:04 ± 19:16 | 91:30 ± 19:29 |
| REM latency (min: sec) | 65:16 ± 21:20 | 68:27 ± 13:34 | 68:24 ± 15:25 |
| Sleep efficiency (%) | 91.6 ± 3.9 | 91.9 ± 3.3 | 92.0 ± 2.2 |
| Non REM Stage 1 (%) | 5.2 ± 3.2 | 5.1 ± 3.3 | 5.2 ± 3.7 |
| Non REM Stage 2 (%) | 53.6 ± 5.4 | 53.5 ± 8.6 | 52.2 ± 6.9 |
| Non REM Stage 3 (%) | 13.8 ± 6.6 | 14.8 ± 8.3 | 13.6 ± 7.9 |
| REM (%) | 26.4 ± 3.6 | 25.8 ± 5.0 | 26.5 ± 5.7 |
| Values are means ± SD, n = 20. Statistics vs. Placebo group by way of repeated ANOVA host hoc bonferroni test, * p < 0.05. REM: Rapid Eye Movement. | |||
An improvement in sleep quality (frequent dreaming) was observed in Japanese middle-aged managers who consumed an edible film containing crocetin for seven consecutive days. Thus, crocetin was demonstrated to have a potential effect on sleep quality, even when administered over a short period of time.
The subjects (50.4 ± 4.8 years old) were characterized by an AIS score of 5.0 ± 3.1 and an ESS score of 10.1 ± 3.6 prior to the study initiation, which was below the cut-off values (AIS ≥ 6; ESS ≥ 13) (Table 3). In a large cohort study of 1,666 corporate employees (649 males and 1,017 females; 45.33 ± 12.20 years), the mean AIS score was reported to be 5.0 ± 3.6 and the mean ESS score was 7.84 ± 4.55; thus, we considered the subjects in our study to be approximately average [28]. The K6 score was 3.1 ± 2.2, which was also below the cut-off (≥ 5). In a previous study of 122 male managers (49.4 ± 5.42 years), the K6 score was reported to be 2.9 ± 3.1 and in a previous study of 168 female managers, the K6 score was reported to be 4.85 ± 4.36 [29,30]. The subjects in the present study were approximately at the same level as those subjects; therefore, our subjects were considered to be representative of the general population. In a study using male workers, it was reported that the work hours of non-managers in Japan had decreased, whereas the workload of managers had increased due to work style changes [31]. Female managers have reported a higher exposure to stress than their male counterparts, both at work and at home [32]. Although managers exhibit higher occupational stress than non-managers, they have been demonstrated to have lower psychological distress. This may, in part, be due to the influence of compensation or rewards from work [30]. For the same reason, the subjects in this study demonstrated an average K6 score and were also considered to have an average score on the AIS.
The results of objective sleep measurement using InSomnograf® revealed no significant differences in sleep parameters such as WASO, sleep efficiency, and the occurrence rates of various sleep stages (Table 5). The percentage of Japanese people in their 40s and 50s who sleep fewer than 7 hours has been reported to be 58% for those in their 40s and 79% for those in their 50s [8]. The percentages of those who sleep fewer than 6 hours have been reported to be 26% for those in their 40s and 38% for those in their 50s. The subjects in this study averaged approximately 6:20 hours lying down and 5:50 hours for the total sleep time, which was approximately the same as or less than the national average. Aging is known to decrease the total sleep time, increase the number of WASO, decrease sleep efficiency, and decrease the occurrence rates of REM sleep and non-REM in sleep stage N₃ [11]. A marked decrease in sleep efficiency is known to occur in people in their 50s and 60s, from 91.4% ± 4.2% for those in their 50s to 80.6% ± 7.9% for those in their 60s [13]. Against this general trend, the sleep efficiency of the subjects in this study (aged 45–63) was approximately 92%, a higher value that indicated no significant decline due to aging (Table 5). Previous studies with crocetin tested those with mild sleep complaints and those with a PSQI of 6 or higher; a decrease in WASO and an increase in delta power were observed [18,19]. By screening people who are dissatisfied with their sleep and using them as test subjects, changes in sleep parameters including WASO, may be observed.
Sleep latency does not significantly vary in age groups from the 20s to the 50s; it has been reported to be 15.9 ± 9.6 minutes in the 50s. In the present study, it averaged fewer than 10 minutes [13], which may suggest the tendency of sleep deprivation. The ratio of REM sleep is reported to be approximately 20% in the 50s; it was slightly higher in this study, at just over 25% [10]. The occurrence rate of stage N₃ non-REM sleep was in line with the average, with the subjects averaging 13.8%; just under 10% has been reported as the average [10]. Stress has been reported to be a possible contributor to an increased rate of REM sleep. Other studies have suggested that stress may also contribute to prolonged sleep latency and increased WASO. In turn, poor sleep quality itself may be a stressor [33]. The magnitude of the effect of stress on sleep is not clear. In the case of this study, occupational stress may have played a role in the high percentage of REM sleep. It is possible that the effect of aging on REM sleep is limited, as no effect was demonstrated on the K6 scores, sleep latency, or WASO. Further investigation of the correlation with stress specific to managers is necessary.
After seven consecutive days of ingestion of an edible film containing crocetin, an improvement in sleep quality (frequent dreaming) was observed (Table 4). A previous study demonstrated an improvement in OSA-MA Factor 3 (frequent dreaming) with food intake; a four-week study of 3,5-dihydroxy-4-methoxybenzyl alcohol (DHMBA)-containing supernatant extracted from the soft tissue of the Pacific oyster (Crassostrea gigas) [34]. The mechanism of action was reported to be the inhibition of arousal due to the lowering effect of plasma corticosterone concentration derived from the reduction in reactive oxygen species in the brain [35]. Antioxidant effects such as activation of superoxide dismutase (SOD) and glutathione peroxidase (GPx) as well as a scavenging activity against hydroxyl radicals have also been reported for crocetin [36]. In vivo, crocetin has been suggested to cross theblood–brain barrier and blood–retinal barrier; its effectiveness in improving eyestrain in humans has been also reported. The correlation between workload and oxidative stress is known; evaluations using the Effort–Reward Imbalance Model have demonstrated that occupational stress and oxidative stress are positively correlated [37,38]. Increases in lectin-like oxidized low-density lipoprotein receptor-1 (LOX-1) and lipid peroxides in the blood have been reported in animal models [39,40]. In this study, crocetin may have crossed the blood–brain barrier in our subjects, contributing to the scavenging of reactive oxygen species in the brain. This antioxidant effect may have reduced plasma corticosterone levels and inhibited arousal, resulting in an improved OSA-MA Factor 3 (frequent dreaming).
It has been suggested that crocin, a water-soluble derivative of crocetin, induces sleep by indirectly inhibiting the wake-regulating function of histamine. In vivo, crocin has been found to exist as crocetin; the functionality of crocetin may increase delta power by inhibiting histamine. Other elements affected with crocin were also observed in OSA-MA Factors 1 (sleepiness on waking) and 4 (recovery from fatigue), all of which suggested the possibility of an increased depth of non-REM sleep [19]. Delta power is one biomarker of non-REM sleep depth; the activation of delta power is thought to result from adenosine acting on the cholinergic nuclei of the basal forebrain, reducing the cholinergic tone that inhibits nerve firing [41]. The detailed mechanism of the action of crocetin on delta power remains unclear. In the present study, there were no significant differences in OSA-MA Factors 1 (sleepiness on waking) and 4 (recovery from fatigue), nor in the duration and percentages of non-REM sleeps measured by InSomnograf® (Tables 4,5). One difference from prior research is that those studies were conducted using subjects with mild sleep complaints and a PSQI of 6 or higher. In addition to the depth of non-REM sleep, delta power has been used as a biomarker for sleep requirement (sleepiness) and is related to sleep debt. It is hoped that the future screening and testing of subjects taking sleep debt into account will elucidate the mechanism by which crocetin causes changes in delta power [42,43].
The following points are limitations of this study. The study was conducted on Japanese middle-aged and older adults (45 and 70 years old). The number of subjects was 20, and the subjects' areas of residence and occupations were rather limited. The subjects were a group that did not have sleep anxiety. The subjects' oxidative stress status was not measured. In order to provide more generalized evidence for the effects of crocetin in the future, we believe that a large-scale study with more than 100 subjects is needed, covering a wide range of ages, residential areas, and occupations. In addition, monitoring the oxidative stress status of the subjects and comparing the results of the studies in groups with and without sleep disorders would play a major role in understanding the effects of crocetin.
In this study, an improvement in sleep quality (frequent dreaming) was observed in Japanese middle-aged managers who consumed an edible film containing crocetin for seven consecutive days. Its application as an active ingredient in sleep supplements will be expanded in the future.
The authors would like to express their appreciation to the subjects who participated in the study.
Author contributions
Conceptualization: HM, KI, TK and MY; Methodology: HM, SN, KI, TK; Formal Analysis: HM, SN; Investigation: YO, SN, CT, KI; Data Curation: HM, SN and TK; Writing – Original Draft Preparation: YO and HM; Writing – Review & Editing: SN, KI, MY, TK; Supervision: KI; Project Administration: KI, TK.
Funding
The study was conducted with funding from Calbee, Inc., Tokyo, Japan. This study was commissioned by Calbee Inc. to S'UIMIN Inc.
Conflicts of interest: YO, HM, and KI are employees of Calbee, Inc. MY is a founder and CEO, TK is a CSO, and SN, and CT are employees of S’UIMIN Inc.
- Kim K, Uchiyama M, Okawa M, Doi Y, Oida T, Minowa M, Ogihara R. Lifestyles and sleep disorders among the Japanese adult population. Psychiatry Clin Neurosci. 1999 Apr;53(2):269-70. doi: 10.1046/j.1440-1819.1999.00547.x. PMID: 10459708.
- Furihata R, Uchiyama M, Takahashi S, Suzuki M, Konno C, Osaki K, Konno M, Kaneita Y, Ohida T, Akahoshi T, Hashimoto S, Akashiba T. The association between sleep problems and perceived health status: a Japanese nationwide general population survey. Sleep Med. 2012 Aug;13(7):831-7. doi: 10.1016/j.sleep.2012.03.011. Epub 2012 May 19. PMID: 22609021.
- Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, Lombardo C, Riemann D. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011 Dec;135(1-3):10-9. doi: 10.1016/j.jad.2011.01.011. Epub 2011 Feb 5. PMID: 21300408.
- St-Onge MP. The role of sleep duration in the regulation of energy balance: effects on energy intakes and expenditure. J Clin Sleep Med. 2013 Jan 15;9(1):73-80. doi: 10.5664/jcsm.2348. PMID: 23319909; PMCID: PMC3525993.
- Pase MP, Himali JJ, Grima NA, Beiser AS, Satizabal CL, Aparicio HJ, Thomas RJ, Gottlieb DJ, Auerbach SH, Seshadri S. Sleep architecture and the risk of incident dementia in the community. Neurology. 2017 Sep 19;89(12):1244-1250. doi: 10.1212/WNL.0000000000004373. Epub 2017 Aug 23. PMID: 28835407; PMCID: PMC5606917.
- Chen Y, Tan F, Wei L, Li X, Lyu Z, Feng X, Wen Y, Guo L, He J, Dai M, Li N. Sleep duration and the risk of cancer: a systematic review and meta-analysis including dose-response relationship. BMC Cancer. 2018 Nov 21;18(1):1149. doi: 10.1186/s12885-018-5025-y. PMID: 30463535; PMCID: PMC6249821.
- Shinto T, Tahara Y, Watabe A, Makino N, Tomonaga M, Kimura H, Nozawa Y, Kobayashi K, Takahashi M, Shibata S. Interaction effects of sex on the sleep loss and social jetlag-related negative mood in Japanese children and adolescents: a cross-sectional study. Sleep Adv. 2022 Sep 21;3(1):zpac035. doi: 10.1093/sleepadvances/zpac035. PMID: 37193406; PMCID: PMC10104387.
- Ministry of Health, Labour and Welfare. Report on the results of the Health Status Survey 2021. https://www.mhlw.go.jp/english/wp/wp-hw14/index.html
- Mander BA, Winer JR, Walker MP. Sleep and Human Aging. Neuron. 2017 Apr 5;94(1):19-36. doi: 10.1016/j.neuron.2017.02.004. PMID: 28384471; PMCID: PMC5810920.
- Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004 Nov 1;27(7):1255-73. doi: 10.1093/sleep/27.7.1255. PMID: 15586779.
- Boulos MI, Jairam T, Kendzerska T, Im J, Mekhael A, Murray BJ. Normal polysomnography parameters in healthy adults: a systematic review and meta-analysis. Lancet Respir Med. 2019 Jun;7(6):533-543. doi: 10.1016/S2213-2600(19)30057-8. Epub 2019 Apr 18. PMID: 31006560.
- Floyd JA, Janisse JJ, Marshall Medler S, Ager JW. Nonlinear components of age-related change in sleep initiation. Nurs Res. 2000 Sep-Oct;49(5):290-4. doi: 10.1097/00006199-200009000-00008. PMID: 11009124.
- Hirasawa H, Atsumi Y. [Polysomnographic changes in normal human aging]. Nihon Ronen Igakkai Zasshi. 1997 Jun;34(6):453-60. Japanese. doi: 10.3143/geriatrics.34.453. PMID: 9301259.
- Ministry of Health Labour and Welfare. Basic Survey on Wage Structure 2022. https://www.mhlw.go.jp/toukei/list/chinginkouzou.html.
- Nakata A, Haratani T, Kawakami N, Miki A, Kurabayashi L, Shimizu H. Sleep problems in white-collar male workers in an electric equipment manufacturing company in Japan. Ind Health. 2000 Jan;38(1):62-8. doi: 10.2486/indhealth.38.62. PMID: 10680312.
- Boyce CJ, Oswald AJ. Do people become healthier after being promoted? Health Econ. 2012 May;21(5):580-96. doi: 10.1002/hec.1734. Epub 2011 Apr 19. PMID: 21506192.
- Sekine M, Chandola T, Martikainen P, Marmot M, Kagamimori S. Work and family characteristics as determinants of socioeconomic and sex inequalities in sleep: The Japanese Civil Servants Study. Sleep. 2006 Feb;29(2):206-16. doi: 10.1093/sleep/29.2.206. PMID: 16494089.
- Kuratsune H, Umigai N, Takeno R, Kajimoto Y, Nakano T. Effect of crocetin from Gardenia jasminoides Ellis on sleep: a pilot study. Phytomedicine. 2010 Sep;17(11):840-3. doi: 10.1016/j.phymed.2010.03.025. PMID: 20537515.
- Umigai N, Takeda R, Mori A. Effect of crocetin on quality of sleep: A randomized, double-blind, placebo-controlled, crossover study. Complement Ther Med. 2018 Dec;41:47-51. doi: 10.1016/j.ctim.2018.09.003. Epub 2018 Sep 8. PMID: 30477864.
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL, Walters EE, Zaslavsky AM. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002 Aug;32(6):959-76. doi: 10.1017/s0033291702006074. PMID: 12214795.
- Furukawa TA, Kawakami N, Saitoh M, Ono Y, Nakane Y, Nakamura Y, Tachimori H, Iwata N, Uda H, Nakane H, Watanabe M, Naganuma Y, Hata Y, Kobayashi M, Miyake Y, Takeshima T, Kikkawa T. The performance of the Japanese version of the K6 and K10 in the World Mental Health Survey Japan. Int J Methods Psychiatr Res. 2008;17(3):152-8. doi: 10.1002/mpr.257. PMID: 18763695; PMCID: PMC6878390.
- Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991 Dec;14(6):540-5. doi: 10.1093/sleep/14.6.540. PMID: 1798888.
- Takegami M, Suzukamo Y, Wakita T, Noguchi H, Chin K, Kadotani H, Inoue Y, Oka Y, Nakamura T, Green J, Johns MW, Fukuhara S. Development of a Japanese version of the Epworth Sleepiness Scale (JESS) based on item response theory. Sleep Med. 2009 May;10(5):556-65. doi: 10.1016/j.sleep.2008.04.015. Epub 2008 Sep 27. PMID: 18824408.
- Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens Insomnia Scale: validation of an instrument based on ICD-10 criteria. J Psychosom Res. 2000 Jun;48(6):555-60. doi: 10.1016/s0022-3999(00)00095-7. PMID: 11033374.
- Okajima I, Nakajima S, Kobayashi M, Inoue Y. Development and validation of the Japanese version of the Athens Insomnia Scale. Psychiatry Clin Neurosci. 2013 Sep;67(6):420-5. doi: 10.1111/pcn.12073. Epub 2013 Aug 5. PMID: 23910517.
- Seol J, Lee J, Park I, Tokuyama K, Fukusumi S, Kokubo T, Yanagisawa M, Okura T. Bidirectional associations between physical activity and sleep in older adults: a multilevel analysis using polysomnography. Sci Rep. 2022 Sep 13;12(1):15399. doi: 10.1038/s41598-022-19841-x. PMID: 36100642; PMCID: PMC9470065.
- Yamamoto YTM, Yamazaki K, Shirakawa S, Azumi K. Standardization of revised version of OSA sleep inventory for middle age and aged. Brain Sci Mental Disorders. 1999; 10:401-9.
- Okajima I, Miyamoto T, Ubara A, Omichi C, Matsuda A, Sumi Y, Matsuo M, Ito K, Kadotani H. Evaluation of Severity Levels of the Athens Insomnia Scale Based on the Criterion of Insomnia Severity Index. Int J Environ Res Public Health. 2020 Nov 26;17(23):8789. doi: 10.3390/ijerph17238789. PMID: 33256097; PMCID: PMC7730071.
- Isojima MKR, Takahashi M, Kiyotaki S, Fukuda M, Mizukoshi M, Araki H, Oshima Y, Iida D, Tanaka K. Effects of coaching skills training by occupational health staff on improving managers’ communication behavior: a randomized controlled trial. Kitasato Medical Society. 2018; 48(2):96-104.
- Shiraki N, Doki S, Ikeda Y, Ikeda T, Takahashi T, Andrea CS, Hori D, Oi Y, Sasahara SI, Matsuzaki I. Differences in psychological distress between managers and non-managers in female workers: a cross-sectional study in Tsukuba Science City, Japan. Nagoya J Med Sci. 2021 Feb;83(1):63-74. doi: 10.18999/nagjms.83.1.63. PMID: 33727738; PMCID: PMC7938094.
- Tanaka H, Nusselder WJ, Bopp M, Brønnum-Hansen H, Kalediene R, Lee JS, Leinsalu M, Martikainen P, Menvielle G, Kobayashi Y, Mackenbach JP. Mortality inequalities by occupational class among men in Japan, South Korea and eight European countries: a national register-based study, 1990-2015. J Epidemiol Community Health. 2019 Aug;73(8):750-758. doi: 10.1136/jech-2018-211715. Epub 2019 May 29. PMID: 31142611; PMCID: PMC6678055.
- Umeda M, McMunn A, Cable N, Hashimoto H, Kawakami N, Marmot M. Does an advantageous occupational position make women happier in contemporary Japan? Findings from the Japanese Study of Health, Occupation, and Psychosocial Factors Related Equity (J-HOPE). SSM Popul Health. 2015 Oct 26;1:8-15. doi: 10.1016/j.ssmph.2015.09.002. PMID: 29349116; PMCID: PMC5757939.
- Slavish DC, Asbee J, Veeramachaneni K, Messman BA, Scott B, Sin NL, Taylor DJ, Dietch JR. The Cycle of Daily Stress and Sleep: Sleep Measurement Matters. Ann Behav Med. 2021 May 6;55(5):413-423. doi: 10.1093/abm/kaaa053. PMID: 32756869; PMCID: PMC8248482.
- Watanabe MTK, Takahashi M, Aramaki N, Horie H, Saito J. Effect of Intake of Jelly Compounded with 3,5—dihydroxy—4—methoxybenzyl Alcohol(DHMBA)—containing Supernatant Extracted from Soft Tissue of the Pacific Oyster (Crassostrea gigas)on Fatigue in Healthy Middle—aged Men and Women ―Randomized, Double—blind, Placebo—controlled, Comparative Study―. Japanese Pharmacology and Therapeutics. 2018; 46(3):383-91.
- Watanabe M KK, Yoshiike K, Aramaki N. The effects of 3,5-dihydroxy-4-methoxybenzyl alcohol (DHMBA)-containing fraction isolated from soft tissue of the Pacific oyster (Crassostea gigas) on sleep electroencephalogram in stressed rats. The journal of Japan Mibyou Association. 2021; 27(1):1-8.
- Shen XC, Qian ZY. Effects of crocetin on antioxidant enzymatic activities in cardiac hypertrophy induced by norepinephrine in rats. Pharmazie. 2006 Apr;61(4):348-52. PMID: 16649553.
- Watanabe S, Li YS, Kawasaki Y, Kawai K. [Workers' Lifestyles and Urinary 8-hydroxydeoxyguanosine as an Oxidative Stress Marker]. J UOEH. 2019;41(4):431-436. Japanese. doi: 10.7888/juoeh.41.431. PMID: 31866661.
- Takaki J. Associations of job stress indicators with oxidative biomarkers in Japanese men and women. Int J Environ Res Public Health. 2013 Dec 2;10(12):6662-71. doi: 10.3390/ijerph10126662. PMID: 24317383; PMCID: PMC3881133.
- Andersson IJ, Sankaralingam S, Davidge ST. Restraint stress up-regulates lectin-like oxidized low-density lipoprotein receptor-1 in aorta of apolipoprotein E-deficient mice. Stress. 2010 Sep;13(5):454-60. doi: 10.3109/10253891003758901. PMID: 20666645.
- Kang DH, McCarthy DO. The effect of psychological stress on neutrophil superoxide release. Res Nurs Health. 1994 Oct;17(5):363-70. doi: 10.1002/nur.4770170507. PMID: 8090947.
- Rainnie DG, Grunze HC, McCarley RW, Greene RW. Adenosine inhibition of mesopontine cholinergic neurons: implications for EEG arousal. Science. 1994 Feb 4;263(5147):689-92. doi: 10.1126/science.8303279. Erratum in: Science 1994 Jul 1;265(5168):16. PMID: 8303279; PMCID: PMC3612520.
- Asai A, Nakano T, Takahashi M, Nagao A. Orally administered crocetin and crocins are absorbed into blood plasma as crocetin and its glucuronide conjugates in mice. J Agric Food Chem. 2005 Sep 7;53(18):7302-6. doi: 10.1021/jf0509355. PMID: 16131146.
- Shah KA, Li G, Song L, Gao B, Huang L, Luan D, Iqbal H, Cao Q, Menaa F, Lee BJ, Alnasser SM, Alshahrani SM, Cui J. Rizatriptan-Loaded Oral Fast Dissolving Films: Design and Characterizations. Pharmaceutics. 2022 Dec 1;14(12):2687. doi: 10.3390/pharmaceutics14122687. PMID: 36559181; PMCID: PMC9780891.